Source: Wikimedia commons Baedr-9439
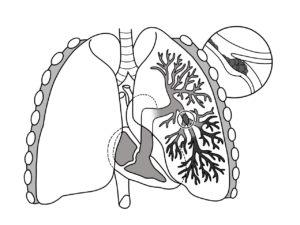
Pulmonary embolism (PE) is a condition in which an artery in the lungs gets blocked by a blood clot.
The most common cause of the formation of embolus usually in the lower extremity is deep vein thrombosis (DVT). PE occurs when a small embolus breaks off from a large thrombus and travels to the lungs where it causes life-threatening blockage.
CAUSES
- Pulmonary embolism occurs: when blood collects in a certain part of the body (usually an arm or leg) which moves through the bloodstream and becomes lodged in the blood vessel of the lungs which restricts blood flow to the lungs, lowers oxygen levels in the lungs, and increases blood pressure in the pulmonary arteries
- Blockages in the blood vessels are also caused by substances such as -: Fat from the marrow of a broken long bone, part of a tumor, air bubbles
Anyone can develop blood clots and which may lead to pulmonary embolism, but certain factors can increase the risk :
- Heart disease -cardiovascular diseases including congestive heart failure, atrial fibrillation, and heart attack or stroke. Increases clot formation.
- Cancer – Certain types of cancers like ovarian, brain, pancreas, stomach, lung, kidney, etc. Chemotherapy and in some women taking hormone replacement therapy or birth control pills can elevate the clotting factors in the blood.
- Surgery- is one of the leading causes of blood clots. For this, medication to prevent clots may be given before and after major surgery, such as joint replacement.
- Disorders-.Some inherited disorders affect the blood, making it more prone to clot. Other disorders such as kidney disease can also increase the risk of blood clots.
SYMPTOMS
Symptoms of pulmonary embolism vary greatly, depending on how much the lung is involved, the size of the clots, and whether one has an underlying lung or heart disease.
Common symptoms like :
- Sudden shortness of breath — whether active or at rest.
- Sharp pain in the chest, arm, shoulder, neck, or jaw. The pain may be similar to symptoms of a heart attack.
- Cough with or without bloody sputum (mucus).
Other symptoms :
- Pale, clammy, or bluish-colored skin.
- Irregular/Rapid heartbeat.
- Excessive sweating.
- Feeling anxious, light-headed, fainting, or passing out.
- Wheezing
DIAGNOSIS
The following tests can be done to diagnose pulmonary embolism:
Blood Test: It helps to determine the amount of CO2 or oxygen in the blood as well as help to detect a substance called D-dimer, a clot-dissolving substance.
Chest X-ray: They can help to eliminate the conditions that resemble pulmonary embolism.
Ultrasound: It determines blood flow & the structure of the blood vessels in the legs. It uses sound waves to scan for vein blood clots.
CT pulmonary angiography: A computerized tomography pulmonary angiography (CTPA) method in which a dye is injected that helps to show the blood vessels. It generates X-rays to create 3-D images of the body.
Ventilation-perfusion scan: Used to examine the flow of air and blood in the lungs with the use of a radioactive tracer material & helps to show which parts of the lungs are getting airflow & blood flow.
Pulmonary angiogram: Gives a better understanding of the blood flow in the arteries of the lungs and is also the most accurate method. A special dye is injected into the catheter & X-rays are taken as the dye travels through the arteries.
MRI: A detailed image of the tissues & organs is created with the use of a magnetic field & computer-generated radio waves.
Echocardiogram: This test cannot detect pulmonary embolism but can spot the areas of the heart with abnormalities. Ultrasound can help to show if the heart is strained.
Electrocardiogram: The electrical activity of the heart is measured, recorded, & interpreted. The test results will help to eliminate possible heart attacks.
Arterial Blood Gas: It measures the blood oxygen level of the sample which is directly taken from the artery with the help of a needle or catheter. The oxygen & CO2 are measured by an arterial blood gas in terms of partial pressures in units of mm Hg.
Spiral Computed Tomography of the Chest: This technique obtains multiple cross-sectional X-ray images of the tissues & organs of the chest. The x-ray machine scans the body in a spiral path. An iodine dye is generally administered into the vein to make the blood vessels distinct.
Genetic predisposition is developing a particular disease based on genetic makeup. Specific genetic variation inherited from a parent contributes to an individual’s disease risk, each individual has a unique set of genes that impact clinical biomarkers and contribute to the expression of common conditions such as heart disease, diabetes, obesity, and hypertension.
PE is a hypercoagulable disorder, for coagulation, there is a need for a particular type of procoagulant enzyme including thrombin factor ten (FX), factor twelve (FXII), factor seven (FVII), factor five (FV). Human factor V is also known as proaccelerin/ coagulation factor V/ labile factor. Factor V Leiden (FVL) is a specific genetic mutation that leads to hypercoagulability and increased risk of venous thromboembolism (including DVT & PE) in individuals who carry the FVL variant. FVL is associated with a thrombophilic state as well as with inflammatory conditions in various disorders. FVL is initially described as APC (activated protein C) resistance, resistance to APC may lead to the development of more extensive blood clots which lead to an increased risk of PE.
FVL increases in procoagulant activity but there is a particular enzyme that breaks down embolus. Enzymes like protein C & S are vitamin K-dependent plasma proteins and natural anticoagulants which work together to prevent abnormal blood clotting. Inhibition of anticoagulant enzymes, decreasing their ability to function, and deficiency of protein C & S would be potential issues. Since these conditions are inherited, individuals need a protein C & S test which is done with blood samples. Test results are used to help diagnose the cause of venous thromboembolism (VTE). Test results can be affected by surgery, pregnancy, and some medicine including blood thinners & birth control pills.
Dietary Management & Lifestyle on Pulmonary Embolism
A pulmonary embolism (PE) happens when a blood clot becomes trapped in a pulmonary artery, cutting off blood supply to a portion of the lung. There is no special diet for PE; nonetheless, doctors advocate eating a balanced diet to avoid conditions that can cause clots.
Foods to be consumed
To guarantee optimal nutrition, a variety of meals such as lean meats like chicken, fatty fish, whole grains like oats, fruits like apples, and a variety of vegetables should be consumed. Antioxidants called phenols in virgin olive oil helped prevent blood clots.
Foods to stay away from
Warfarin (a drug used to prevent blood clotting) can be made more potent by cranberry products like juice, which might lead to bleeding issues. One should avoid eating cranberries and drinking cranberry juice if they have a pulmonary embolism and are taking warfarin. Warfarin’s efficacy is also impaired by alcohol and licorice. Unhealthy trans fats, from the saturated fats in full-fat dairy and fatty meats, and from all types of sugar can increase inflammation.
Vitamin K can reduce the effectiveness of warfarin. Elimination of vitamin K completely from the diet can lead to bleeding or clotting. Therefore, it is recommended that for patients to consume moderate vitamin K on a regular basis. Kale, broccoli, leafy green vegetables, and soy products are high in vitamin K.
If someone has a higher risk of PE, a customized plan with the doctor is discussed to lower the risk. There are some lifestyle adjustments that may be part of their plan.
- Consumption a well-balanced diet to achieve and maintain a healthy weight and lower your risk of blood clots.
- To prevent blood pooling in the legs, raise their feet for 30 minutes twice a day.
- To avoid blood pooling, one should exercise regularly and move their legs. Move arms and legs for a few minutes every hour if they are bedridden or sit for lengthy durations. Once or twice a day, take a walk around the block or down the driveway. Also, to help the blood flow faster, avoid crossing your legs while sitting.
- To avoid dehydration and to get them up and moving, drinking plenty of water and juice (to the bathroom) is recommended. Caffeine and alcohol should be avoided in excess.
- Avoid smoking or get help to quit.
- Compression stockings are worn to assist avoid leg edema and blood clotting.
- Stretching of arms and legs if they can’t stand up or if they have been sitting for a long time to maintain blood flowing freely. Those traveling more than 4 hours by air, by car, or by bus can be at risk for blood clots.
- If they’re overweight, exercise, aim to lose weight, and maintain a healthy weight.
All in all a greater understanding of PE helps both the patient and the clinician to manage the disease optimally.
The author acknowledges the use of authentic medical literature to structure this article.
Sign up for the QuackTrack.org newsletter below!