Liposuction by Nick Youngson CC BY-SA 3.0 Alpha Stock Images
When choosing a line of treatment, surgery and surgical procedures are viewed even to this day with a great deal of caution. The procedure or technique per se may be perfected and well-executed by a trained surgeon, however, the subsequent response of the patient’s biochemical profile, post the procedure are quite individual. This response is generally termed as postoperative trauma and is governed by several factors.
Perioperative medicine governs the road to wellness and good health and is still an area of dynamic research and always contributes to the overall success of the surgery. Many surgery-oriented procedures are termed as dispensable and elective and the patient is suggested alternative methods of treatment by the medical expert.
In reality, the very synonymous term for surgery is “Invasive Procedure”……that which disturbs the original make-up of the body organization. Hence, coming to the point of this article, Liposuction, one needs to view this area of Invasive surgery with a broad assessment of pros and cons. My endeavor would be to place before the reader a wide plethora of perspectives with no view of being either judgemental or biased about Liposuction.
Liposuction- History and Development
Liposuction, also known as Lipoplasty is a surgical methodology where adipose tissues of the body are addressed and the lipid molecules or fat is removed through suction. Simply called lipo, it is a cosmetic surgery performed to remove fat from areas where fat usually accumulates such as the abdomen, thighs, back of arms, etc.
Societal definitions of good looks are unquestionably associated with slim bodies.
In both genders, there is a universal opinion that lithe, appropriately curvaceous human forms are coveted, at the same time this target is many times difficult to achieve and maintain. Diets are like lifestyle changes, gyms and exercises are tiresome both literally and figuratively and the dream figure is quite far beyond one’s horizon.
Hence, quick fixes like liposuction are often ways of achieving the ‘desirable figure’. Some individuals do not ‘like’ a part of their body and are happy to change nature’s handiwork at the surgeon’s table and under his knife.
A loud and clear message from my side would be to ‘read the small print’ and weigh out the options before any such ‘Elective Surgery’ is performed more so because it is not mandatory but by choice.
Historical facts and revelations about Liposuction are sketchy and if the progress were to be plotted graphically, one can certainly expect an undulating and wavy graph. In the 1920s, Charles Dujarier performed the first Liposuction in France.
However, the horrific final result was the removal of the leg since the amount of tissue sacrificed was excessive and caused gangrene. All this in the case of a dancer would you believe?! The print media went to a party on this ‘failure’. They coined the word ‘Body Contouring’ and even called it the work of Satan’s wedge knife. The consequence was that for almost four decades, there was a projected peace and quiet in this area of surgical sciences.
Importantly, the contribution of Dr. Arpad and Dr. Giorgio Fischer to the evolution of Liposuction around the 1970s cannot be ignored. The father-son duo developed the blunt tunneling instrument called a cannula after which modern liposuction evolved. Sometime later another surgeon Pierre Fournier Illouz introduced the use of lidocaine as a local anesthetic laying the groundwork for the tumescent technique used today.
In the late 1990s, doctors introduced the use of ultrasound to make removal of the adipose tissue more effective.
Around that era of medical history, there were various inventions in devices and machines for use in curative practice and above all the use of radiation, scanning procedures and even mechanical gadgetry was the order of the day.
With so much equipment at hand and surgeons becoming more and more confident of their use, surgery was now being viewed as hugely doable and with definite success.

Pexels. Public domain
Naturally, many surgeries and invasive procedures were looked into as what was believed to be ‘aesthetic purposes’, and Plastic surgery was in its golden period.
Cosmetic Surgery was frequently resorted to by various individuals from celebrities and people in the limelight to common people who were driven to convert “better’ to “best”.
Of course, in the general thought process of one and all, the hourglass figure was endorsed and appreciated as the signature of beauty. It is, therefore, no surprise that a study carried out in the US, found that surgical procedures for the augmentation of breasts came a poor second to Liposuction…..the year was 2015!
If one were to delve into the classification and projected convenience of Liposuction, there are two aspects that are common.
First, the procedure is resorted to in the face of an absolutely mandatory requirement by the expert or, second when Liposuction is diametrically opposite….It may be for purely cosmetic reasons and in that sense can be considered dispensable and elective.
Depending on the specific details, the patient is subjected to general, regional, or local anaesthesia and the surgery is then performed. Additionally, the time taken for the completion of the surgery varies from case to case.
Liposuction Procedure and Risks
On paper, the procedure of Liposuction seems very simple and easy to conduct.
A cannula or thin tube is used and suction pressure is applied, using an aspirator, to suck out the fat from that particular area of the body. If the subject undergoing surgery does not have any comorbidity, has skin elasticity which is optimal and if his BMI (Body Mass Index) is normal, there are more chances of a successful Liposuction.
As I said before in the article, there is a lot of small print and the flipside is quite heavy. These have to be understood and taken with appropriate seriousness.
Some shocking aspects of the aftermath of liposuction…if the fat is removed from around the visceral organs during the procedure, there is a large likelihood of manifestation of diseases like hypothermia, diabetes, hypertension, and CVD(cardiovascular disease).
In rare cases, a condition such as fat embolism syndrome (FES), can develop where fat travels through the body and blocks blood vessels
One should remember, that fat is nature’s own lubricant and also serves as a protective layer for the abdominal organs.
Additionally, the fat cells which are removed during liposuction would not come back, but studies have shown that there is an overall tendency of the body to regain the lost ‘weight of the cells’, in a few days’ time. An important aspect to consider is that in a condition like insulin resistance, which is governed by metabolic undertones, liposuction does not help the clinically morbid obesity condition at all.
Is Liposuction Medically Necessary?
In those cases where liposuction is needed as an extrapolation of other clinical diseases, the term medically mandatory Liposuction is used.
Lymphedema (simply defined as a swelling in the limbs because of dysfunction in the flow of lymph fluids) and lipomas or malignancies (tumors) require the excess fat to be removed for the curative efficacy of the primary disease condition. Such surgery is in keeping with medical ethics.
Studies have shown that liposuction also helps patients with Lipoedema ( another medical disorder defined as an abnormal build-up of fat cells,) and it is mostly a female condition.
Liposuction is also used to treat Gynecomastia, a condition where excess fat accumulates under a man’s breasts.
Liposuction is used to remove Lipomas. Lipomas are benign tumors of mature fat cells.
How much liposuction is ‘safe’?
The answer to what’s a safe amount of fat to remove always depends on the patient’s body mass index (BMI).
A frequent query by one and all is what exactly would be the limit to the maximum reduction in weight for the procedure still to be is truly safe? In answer, if there is a removal of fat which may be in the range of six to about eight pounds equivalent to a volume from three to four liters then this would still keep liposuction in the GRAS category(Generally Regarded as Safe). However, if the amount of fat removed in a single day would be more, the risk would also increase.
The frequency of undergoing liposuction for cosmetic purposes also draws multiple responses from medicos. Till the body totally recovers from the previous invasion, the next procedure is generally not recommended.
Liposuction Methods.
The methodology of conduction of Liposuction is variable and various techniques are available many of which are patented. Lasers, ultrasound, power, and water jets are used as assisting components. Fat freezing techniques are also used.
Tumescent liposuction:
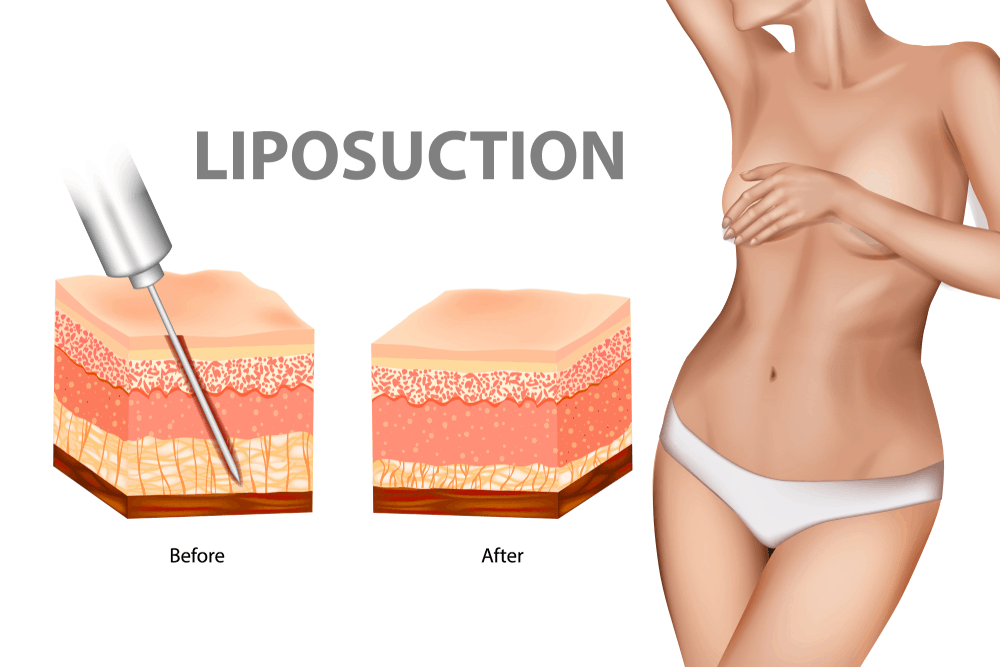
This is the most common form of liposuction that is relatively safer, and less painful. This method is used to remove lipomas, and to treat enlarged male and female breasts. A local anesthetic (lidocaine) and a drug called epinephrine are injected into the fatty area that is to be suctioned. The fat is then sucked out, through small skinny suction tubes that are connected to a vacuum-like machine.
Dry liposuction:
This is performed under general anesthesia. A solution containing local anesthesia is injected into the fat. This method is not used today due to excessive blood loss.
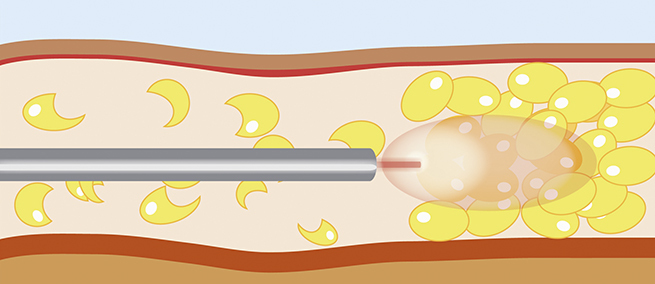
Ultrasound-assisted liposuction (UAL):

Image source: US liposuction
This technique uses waves, to liquefy fat in the area where fat is concentrated. External ultrasound uses a tool to emit sonic vibrations outside the body and through the skin which breaks up the fat and melt. This liquifies the fat making it easier for suction. UAL is suitable for areas, such as male breasts, and back. In this method there is a risk of developing seromas as the heat damages blood vessels and lymphatic vessels, allowing fluid to collect in the fatty tissue.
After ultrasonic liposuction, suction-assisted liposuction is done to remove the liquefied fat.
Power-assisted liposuction (PAS):

Image:Explore plasticsurgery
PAS uses a technique similar to tumescent liposuction. In this method a specialized cannula with a vibrating tip that breaks down deposits of fat with its pulverizing effect. The vibrating tip on the cannula allows the surgeon to speed up the breakdown and pull out fat more easily. There are some minor risks that include skin becoming wrinkled, or uneven but may recover over time.
Laser Assisted Lipolysis (LAL):
source: inter-medic
This method uses laser energy to liquefy fat cells and the procedure requires the use of tumescent fluid to be injected under the skin. A small tube containing a fiber-optic of microns in diameter is inserted through a small incision to deliver laser energy and heat into the fat reaching the adipocytes.
Post-Liposuction Operation and Risks
After the operation, the surgeon may leave the incisions open so that excess fluid and blood can drain from the body.
The post-procedure suturing is a viable point of controversy among medical experts. Some medicos prefer to leave a small gap in the area of invasion or incision to allow the excess fluid drainage. However, this area becomes vulnerable to infection and even sepsis which may be causative to even a life-endangering situation.
Liposuction is a procedure that is projected as a “lunchbreak surgery” and this term is intended to describe its safety.
One should be wary of advertisements that use unqualified superlatives to promote their business. It is very important to know that most of these advertisements are not created to inform you of every possible risk of liposuction.
Various patented Liposuctions project their clean chit, no mortality statistics as their USP (Unique Selling Point). However, it is only fair and ethical to have a frank and holistic patient counseling session, where the family could also be involved. To evaluate the contraindications and dangers of Liposuction, the spectrum of factors involved are numerous.
The patient incumbent has to be mentally prepared for a tangible period of pain and discomfort. This unenviable condition of pain is maybe variable in its intensity and duration from other individuals in the same league.
Some patients even complain of recurrent nagging pain in the affected area for months and even years. Other protracted symptoms post-surgery may include embolism (a simple definition being: Obstruction of a blood vessel, maybe artery or vein due to an air bubble or a clot), bruising, infections, and even vulnerable areas of skin which may get punctured periodically.
As aging continues, the subject may be more prone to accumulation of serum especially in the area of the surgery. Sometimes, skin necrosis, tissue laceration, and nerve transmission impairment are also significant in patients who have undergone liposuction. Scars, deformities, and even toxicity syndrome is expected in some other cases.
There are reports that mortality rates border around one per ten thousand subjects, but clinical reasons which may lead to the loss of life are organ perforations, internal and interstitial hemorrhage or bleeding, deep vein thrombosis, and widespread secondary infection.
A cliché to sum up….
“TREAD SOFTLY….THE ICE IS THIN”
References
- Dixit, VV; Wagh, MS (May 2013). “Unfavourable outcomes of liposuction and their management”. Indian Journal of Plastic Surgery. 46(2): 377–92.
- Seretis, Konstantinos; Goulis, Dimitrios G; Koliakos, Georgios; Demiri, Efterpi (2015). “Short- and Long-Term Effects of Abdominal Lipectomy on Weight and Fat Mass in Females: A Systematic Review”. Obesity Surgery. 25 (10): 1950–8.
- Seretis, K; Goulis, DG; Koliakos, G; Demiri, E (December 2015). “The effects of abdominal lipectomy in metabolic syndrome components and insulin sensitivity in females: A systematic review and meta-analysis”. Metabolism: Clinical and Experimental. 64 (12): 1640–9.
- Norton, Jeffrey A. (2012). Surgery Basic Science and Clinical Evidence. Berlin, Heidelberg: Springer Berlin Heidelberg. p. 2014. ISBN 9783642572821.
- Khan, MH (November 2012). “Update on liposuction: clinical pearls”. Cutis. 90 (5): 259–65.
The author acknowledges the use of authentic medical literature to structure this article.
Also read: Dimpleplasty: for a dent which dazzles
The contents of this article are not meant to be a substitute for medical advice, diagnosis, or treatment, and should not be construed or treated as such. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. We make no representations, warranties, or guarantees, whether express or implied, that the content on our website is accurate, complete, or up to date.
Sign up for the QuackTrack.org newsletter below!