Photo credit: Chuy Gutierrez
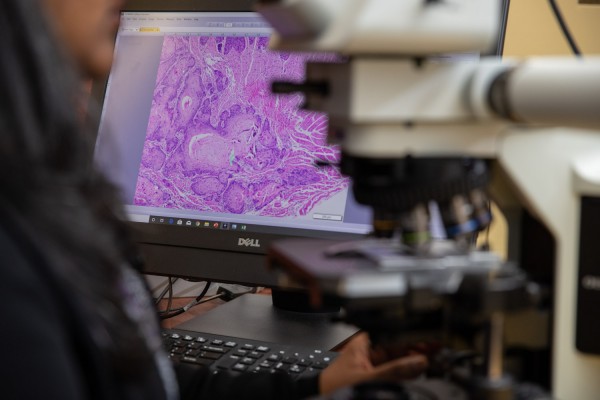
Aditi Bhattacharya, PhD, studies oral cancer using a microscope.
Oral cancer is more likely to spread in patients experiencing high levels of pain, according to a team of researchers at New York University (NYU) College of Dentistry that found genetic and cellular clues as to why metastatic oral cancers are so painful.
The findings—which appear in Scientific Reports, a journal published by Nature—may ultimately be used to alleviate oral cancer pain and refine surgical decision making when treating oral cancer.
Oral cancer can cause severe pain during everyday activities, including talking and eating. Previous research by Brian L. Schmidt, DDS, MD, PhD, director of the NYU Oral Cancer Center and one of the study’s authors, suggests that patients with metastatic oral cancer—cancer that spreads beyond the mouth—experience more pain than those whose cancer has not spread. The new study helps researchers understand why.
When oral cancer metastasizes, spreading to lymph nodes in the neck, a patient’s chance of survival is cut by half. However, it’s often unclear through imaging and physical assessment if oral cancer has spread, leaving surgeons struggling with whether to preemptively remove lymph nodes—an invasive procedure termed prophylactic neck dissection—during surgery to remove the oral cancer. While most oral cancer surgeries include a prophylactic neck dissection, research shows that up to 70 percent are unnecessary.
“Clinicians and researchers are keen to define a biomarker that accurately predicts metastasis,” said Aditi Bhattacharya, PhD, an assistant professor in the Department of Oral and Maxillofacial Surgery at NYU College of Dentistry, an investigator at NYU Bluestone Center for Clinical Research, and the study’s lead author. “Given that patients with metastatic oral cancer experience more pain, we thought that a patient’s level of pain might help predict metastasis. A surgeon could then use this knowledge to only remove lymph nodes in patients with cancers that are most likely to metastasize.”
In their study in Scientific Reports, the researchers first documented the pain experienced by 72 oral cancer patients before surgery, using an oral cancer pain questionnaire developed by the investigators. While most patients reported some pain, those who suffered with the most pain were more likely to have cancer that spread to lymph nodes in the neck. This observation suggests that patients with less pain are at low risk of metastasis, and will rarely benefit from a neck dissection.
To begin to understand why metastatic cancers are more painful, the investigators looked for differences in gene expression between metastatic cancers from patients with high levels of pain compared to non-metastatic cancers from patients not experiencing pain. Cancer pain is attributed to the release of mediators from cancers that sensitize nerves near the cancer. Forty genes were identified that were more highly expressed in painful metastatic cancers, suggesting that they promote metastasis and mediate cancer pain. Many of these genes are found in exosomes, small vesicles that break away from a cell and can be taken up by other cells—revealing a potential mechanism for how cancers communicate with nerves.
“I have been investigating the underlying cause of oral cancer pain for two decades. This is the first time that we have demonstrated a correlation between a patient’s pain and the clinical behavior of the cancer,” said Schmidt, who is also the director of the NYU Bluestone Center for Clinical Research and professor in the Department of Oral and Maxillofacial Surgery at NYU College of Dentistry.
Next, the team undertook laboratory experiments to study exosomes found in the extracellular fluid of oral cancer cells grown in the lab. When this extracellular fluid was injected into animal models, it produced pain, but when the cancer-derived exosomes in the fluid were removed, it did not cause pain. This suggests that exosomes from cancer may be responsible for oral cancer pain.

Research Zinaida Dubeykovskaya performs an assay to characterize the exosomes found in oral cancer. Photo credit: Chuy Gutierrez
Now, with a deeper understanding of why metastatic oral cancers are painful, the researchers point to several potential clinical applications for their research, including a biomarker for oral cancer metastasis to help with surgical decision making and future testing options.
“While we need to undertake a follow-up study, our current data reveal that a patient’s pain intensity score works as well as the current method—depth of invasion, or how deeply a tumor has invaded nearby tissue—as an index to predict metastasis,” said Bhattacharya.
“The identified genes are targets for therapy aimed at stopping pain and cancer. In addition, exosomes shed from cancers can be detected in saliva, blood, and urine, offering the potential for an objective molecular test to diagnose risk of metastasis,” said Donna Albertson, PhD, professor in the Department of Oral and Maxillofacial Surgery at NYU College of Dentistry, an investigator at NYU Bluestone Center for Clinical Research, and the study’s corresponding author.
The research was supported by the National Institutes of Health grants (R01CA113833, R21CA163019, 3UL1TR000004-07S1, R01DE019796, R01DE026806, and R21DE026964).
Sign up for the QuackTrack.org newsletter below!